Tylenol Use During Pregnancy: Examining Research on Autism Risk
Does Tylenol Use during Pregnancy Cause Autism? What the Research Shows
In a press conference this afternoon, the Trump administration linked rising rates of autism spectrum disorder to the use of Tylenol (a brand name of acetaminophen) during pregnancy. “Don’t take it if you’re pregnant. Don’t take Tylenol,” President Trump said, repeatedly emphasizing that pregnant people with fever should “tough it out” as much as they can, despite evidence that uncontrolled fever and infections during pregnancy can themselves increase risk of autism.
This story will be updated as it develops.
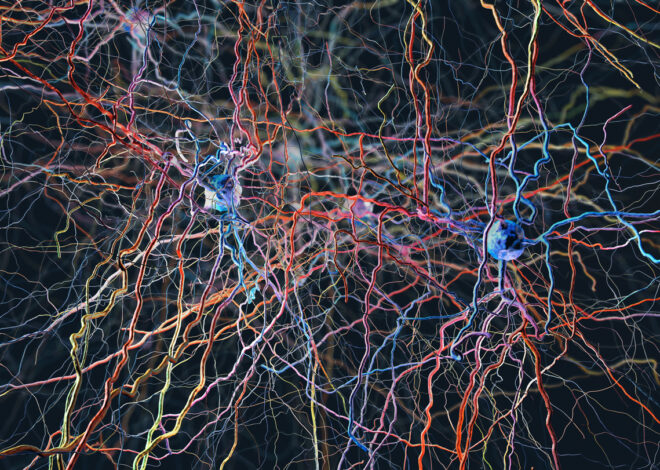
There is no simple answer to what causes autism, more than 50 years of scientific research has shown. It is a complex neurodevelopmental condition that arises from a constellation of genetic factors and environmental influences.
On supporting science journalism
If you’re enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
What’s more, the evidence linking the use of Tylenol during pregnancy to eventual autism diagnoses in children is weak. “The evidence [from a handful of studies] was really mixed, and the effects were really small,” said David Mandell, a professor of psychiatry studying autism at the University of Pennsylvania, in an interview with Scientific American earlier this month.
Acetaminophen is one of the few pain relievers deemed safe to take during pregnancy, in consultation with doctors, according to the American College of Obstetricians and Gynecologists (ACOG). “Today’s announcement by HHS is not backed by the full body of scientific evidence and dangerously simplifies the many and complex causes of neurologic challenges in children. It is highly unsettling that our federal health agencies are willing to make an announcement that will affect the health and well-being of millions of people without the backing of reliable data,” wrote the professional body in a statement sent on Monday to Scientific American.
Here’s what we know about Tylenol and the causes of autism.
What causes autism?
The majority of autism cases can be linked to genetic causes. But that DNA blueprint doesn’t determine everything: as a fertilized human egg turns into an embryo and then into a fetus, environmental factors can influence how those genetic instructions are carried out.
Some nongenetic factors have been repeatedly linked to an elevated risk of developing autism spectrum disorder. The most well-established one is parental age: the older a person’s parents are at the time of that individual’s conception, the more likely it is that that person will be diagnosed with autism. (But even this effect might tie back to genetics because, as people age, they accumulate more genetic mutations that they might pass on to their offspring.)
Other nongenetic factors, such as premature birth or birth by cesarean section, maternal diabetes and exposure to air pollution or certain antiseizure drugs in utero have been shown to increase a person’s risk of autism in some studies. But these results can’t establish that these factors caused the increased risk of autism, only that they sometimes occur together. That’s because it is usually impossible, impractical or unethical to run randomized trials on pregnant populations.
READ MORE: Autism Has No Single Cause. Here’s How We Know
What does the evidence for Tylenol and autism show?
A handful of studies from the U.S. and Europe have found modest increases in autism risk among the offspring of people who took acetaminophen while pregnant. The largest recent study, however, found no effect. The 2024 analysis looked at nearly 2.5 million people born in Sweden between 1995 and 2019. The researchers found a very small increase in the prevalence of autism among the progeny of people who took acetaminophen while they were pregnant compared with the offspring of those who didn’t—the risk was 0.09 percentage points higher. This elevated risk disappeared when researchers just looked at sibling-pair cases in which a person took acetaminophen during one pregnancy and not the other, however. This suggests that what initially looked like an elevated risk of autism from acetaminophen during pregnancy may have been a result of other risk factors.
The most obvious factor that could be influencing these results is the reason people take Tylenol during pregnancy in the first place. The drug is used to relieve pain and to reduce fever. “In none of these studies do I see where [the researchers] were able to separate out the effects of prenatal infection from the acetaminophen use,” Mandell says.
This means that the fever or underlying infections Tylenol was used to treat could be part of what drove the increased risk of autism that was shown in some studies. If a pregnant person is hospitalized with an infection, the likelihood that their child will develop autism increases by approximately 30 percent, a study of more than two million people found.
“In more than two decades of research on the use of acetaminophen in pregnancy, not a single reputable study has successfully concluded that the use of acetaminophen in any trimester of pregnancy causes neurodevelopmental disorders in children,” wrote ACOG in its statement to Scientific American.
“We believe independent, sound science clearly shows that taking acetaminophen does not cause autism. We strongly disagree with any suggestion otherwise and are deeply concerned with the health risk this poses for expecting mothers,” a spokesperson of Kenvue, Tylenol’s manufacturer, said in a separate statement sent to Scientific American.
READ MORE: Tylenol is Popular and Safe, Yet Nobody Knows How it Works
A Potential Treatment
The Trump administration also linked autism to low levels of folate, or vitamin B9, during pregnancy.
“We know that folate deficiency during pregnancy results in neural tube defects or increases risk for neural tube defects,” says Mandell, referring to the structure in an embryo that eventually develops into the brain and spinal cord. “There’s some thought that it could also result in learning disability, developmental delay—including autism.” This idea has led many doctors and parents of people with autism to try treating the condition with B vitamins, including leucovorin, also known as folinic acid.
“Whether folate deficiency affects fetal development is a very different question than ‘Can increasing folate postnatally reduce autism symptoms?’” Mandell says. A few small, randomized controlled trials of folinic acid as a treatment for autism spectrum disorder have been conducted, and they have shown small effects.
“Should we run a large-scale randomized trial of folinic acid and autism? Absolutely. And the reason we should do it is because the science needs to catch up with practice here [because] it’s already being prescribed,” Mandell continues.
Rising rates
Autism rates have been rising, something that Robert F. Kennedy, Jr., frequently refers to as an “epidemic.” The causes of this rise are relatively well known, however. As our understanding of autism has improved, the diagnostic criteria have broadened, and a major change occurred in 2013 when autism and several other conditions were combined into one continuous spectrum disorder in the Diagnostic and Statistical Manual of Mental Disorders. Improved screening is alerting clinicians to more cases in children, and adults whose autism was missed when they were younger are seeking diagnoses. Additionally, improved understanding of autism has allowed for better diagnoses of people who, in prior decades, may have received other diagnoses such as “intellectual disability.”
READ MORE: The Real Reason Autism Rates Are Rising
In April Kennedy said that his Department of Health and Human Services would find the cause of autism by September. But science often does not happen on such short timelines, experts say. The administration’s decision to highlight acetaminophen and folate does not come from new evidence but rather from previously published results that are mixed and point to the need for more research.
“The idea that [the administration] would highlight two things that have such small, controversial and weak evidence is really concerning,” Mandell says—“especially when we know so much about the genetics of autism, and we know so much about other environmental factors that increase the risk for autism.”
“A press statement that talks about a potential association will cause lots of fear,” said Debra Houry, former chief medical officer of the Centers for Disease Control and Prevention, in a press call this morning hosted by the group Defend America Action. Houry participated alongside other former CDC leaders who had resigned this month. “If there is not the science to back it up, we will see practice changes, worried moms, all sorts of things, and that’s not appropriate. You have to be grounded in gold standard science,” she said.
Additional reporting by Lauren Young.
Editor’s Note (9/22/25): This article was updated after posting to include President Trump’s statements from the press conference. Additional statements from Kenvue and the American College of Obstetricians and Gynecologists were also included after posting.
Source:
www.scientificamerican.com
Published on 2025-09-22 17:30:00 by | Category: | Tags: