Breathing device could have profound impact on survival for people with sleep apnea and type 2 diabetes
People with both type 2 diabetes (T2D) and obstructive sleep apnea have a higher risk of death, but treatment with continuous positive airway pressure (CPAP) may reduce that risk by around 26%, according to new research being presented at this year’s Annual Meeting of the European Association for the Study of Diabetes (EASD), Vienna (15–19 Sept).
The Swedish researchers said the results underscore the importance of treating sleep apnea as part of a broader effort to control type 2 diabetes and improve long-term survival.
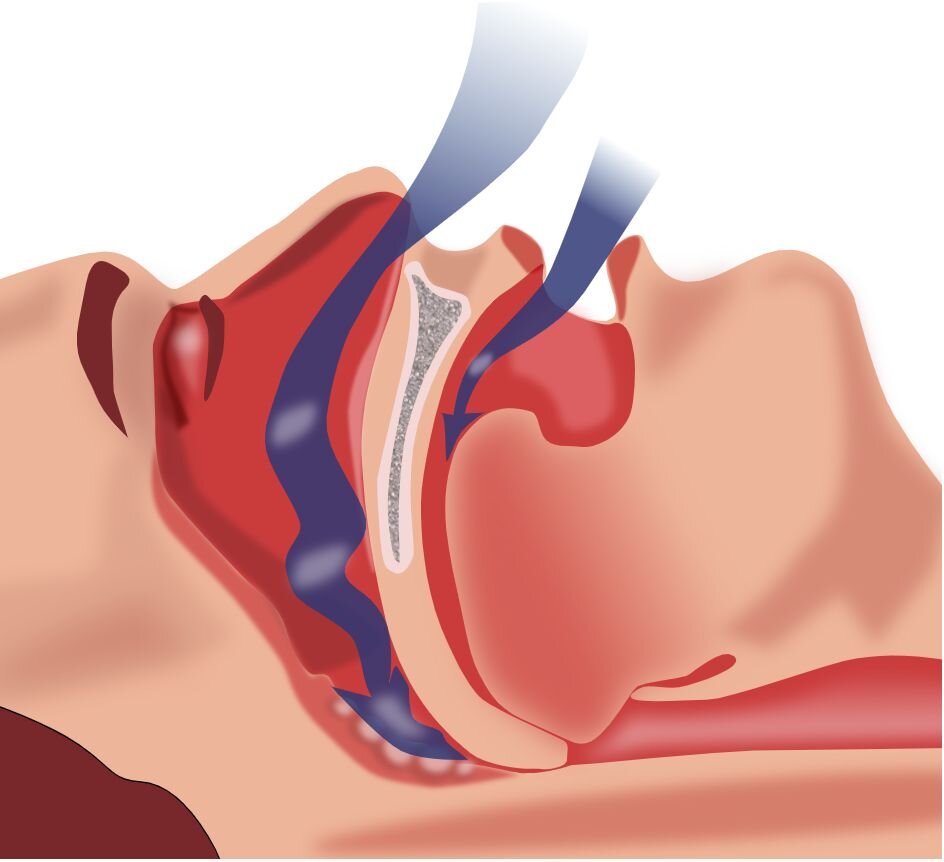
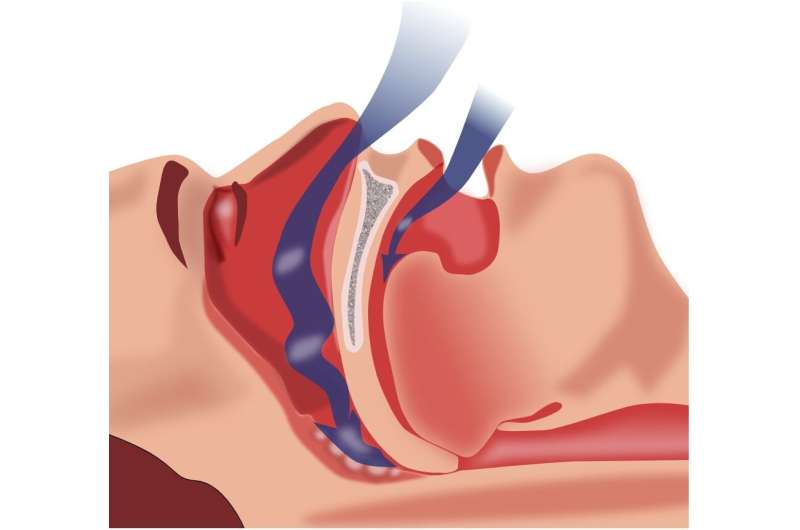
Obstructive sleep apnea is when throat muscles relax during sleep, blocking the airway, causing a person to wake up repeatedly to breathe. This disrupted sleep pattern can lower oxygen levels, affecting the brain. If left untreated, it can lead to serious health problems, including high blood pressure, heart trouble, and T2D.
CPAP machines treat sleep apnea by delivering pressurized air through a mask to keep the airway open during sleep. However, research on the effects of CPAP on survival has produced mixed results.
Obstructive sleep apnea affects around 1 billion of the world’s adults aged 30–69 years, and an estimated 50–80% of adults with T2D, most of whom are undiagnosed, increasing the risk of complications. In people with T2D, sleep apnea is associated with more than a 50% increased risk of cardiovascular disease (including heart failure and stroke) and a 24% higher risk of dying from any cause compared to those without sleep apnea.
“Despite the substantial impact of obstructive sleep apnea on cardiovascular disease and survival, it often goes undiagnosed in people with type 2 diabetes and is not routinely addressed as part of diabetes management,” said lead author Dr. Jonas Aghome from Linköping University in Sweden. “What’s more, the impact of treatment with CPAP on survival in people with T2D hasn’t been clear.”
Previous studies in patients with both T2D and obstructive sleep apnea have been limited by short follow-up periods and a focus on metabolic endpoints, rather than on longer-term clinical outcomes such as survival.
To answer these questions, Swedish researchers analyzed data from five Swedish national registers between 2010 and 2024 to identify 12,388 T2D patients with obstructive sleep apnea who had been prescribed CPAP and 737,911 T2D patients (whose obstructive sleep apnea status was unknown) who were never prescribed CPAP, to compare long-term survival.
Dr. Agholme explains, “Despite potential dilution from including individuals without obstructive sleep apnea in the control group, the high prevalence of obstructive sleep apnea in people with T2D, together with the higher risk of illness associated with having both T2D and obstructive sleep apnea, should allow any clinically relevant associations of CPAP to be detected.”
The CPAP treatment group included fewer women (31% vs. 43%), was younger (average age 58 years vs. 65 years), but had a higher average body mass index (BMI, 34.7 kg/m² vs. 30.6 kg/m²).
Of those prescribed CPAP, 764 people (6.1%) died within 14 years compared to 212,336 people (28.7%) of those who did not receive CPAP.
After adjusting for potential confounders including age, sex, and prior cardiovascular disease, as well as factors that may vary during follow-up including BMI, smoking, cholesterol, kidney function, blood pressure, and pharmacological treatment, they found that patients who were prescribed CPAP had a 26% lower risk of dying from any cause over the 14-year period, compared with patients who never received CPAP.
“This new study using real-world data highlights the potential benefits of CPAP in people with T2D and obstructive sleep apnea, a clinical conundrum that has long awaited answers,” said Dr. Agholme. “The findings suggest that CPAP may play an important role in improving patient outcomes and survival, and they underline the value of early OSA diagnosis in people with T2D. Still, more rigorous research is needed to determine the causal effect of CPAP treatment.”
This is an observational study, and as such, residual confounding and selection bias cannot be entirely ruled out. The authors also acknowledge that data on CPAP adherence were only available for a small subset of patients, so the analyses followed an intention-to-treat principle. They also lacked information on sleep apnea severity across groups, so could not examine whether the effect of CPAP differs by severity.
Finally, since the study was conducted within the Swedish health care system, further work will be needed to assess the generalizability of these findings to other contexts.
Provided by
European Association for the Study of Diabetes
Citation:
Breathing device could have profound impact on survival for people with sleep apnea and type 2 diabetes (2025, September 8)
retrieved 8 September 2025
from https://medicalxpress.com/news/2025-09-device-profound-impact-survival-people.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.